Understanding the principles of time dependent outcomes in tourniquet application.
Driven by experience in both military and civilian trauma care, the liberal and early application of tourniquets has become a universally accepted lifesaving emergency intervention for the pre-hospital management of catastrophic limb haemorrhage.
Within the traditional framework of rapid evacuation times to initial surgical care, arterial tourniquets have proven to be highly effective and consistently safe with low complication rates. However, delivery of future ready medical care within the Australian Defence Force (ADF) needs to consider potential operational environments where the surgical management of limb injuries is delayed for multiple reasons including contested evacuation asset manoeuvre, long evacuation distances, and the capability limitations of lightweight mobile health care facilities.
A limb tourniquet, when applied for an extended duration, creates time dependent tissue damage with impaired functional recovery – decreasing limb viability and ultimately increasing risk of amputation. The challenges associated with the management of casualties using tourniquets in a prolonged field care environment are complex and influence the decisions of both health care providers and commanders. The Tourniquet Traffic Light provides a simplified common framework for understanding time dependent outcomes associated with limb tourniquet application.
The Tourniquet Traffic Light clock starts at the time of injury as blood supply to the limb is first compromised by the initial wounding (Figure 1).
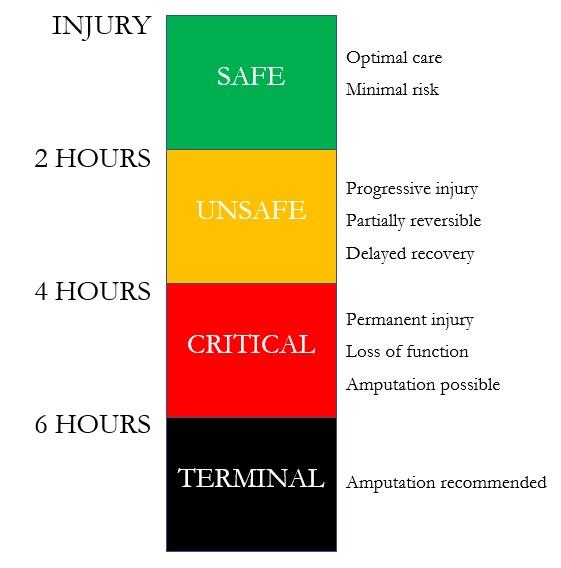
Figure 1: The Tourniquet Traffic Light. Duration of time since injury sustained indicated (left) and description of outcomes and effect (right).
Ideally, tourniquet application time should closely approximate the time of injury in line with contemporary Tactical Combat Casualty Care (TCCC) guidelines. Time after wounding is then broken into progressive 2-hour intervals reflecting increasing risk of injury associated with tourniquet application.
The Tourniquet Traffic Light clock only stops when blood flow to the limb has been restored. This requires both removal of the tourniquet and corrective surgical intervention where necessary. It is important to recognise that any compounding time delay prior to surgical intervention contributes to overall tourniquet risk. Evacuation time therefore needs to consider not only transportation but also delays which routinely occur at the destination facility such as transport from an air head, receiving facility triage, emergency resuscitation, and delays in conducting corrective surgical intervention such as the care of higher priority casualties or in the management of higher priority injuries presenting within the same casualty.
With appropriate application techniques, arterial tourniquets applied for less than 2 hours duration are safe (Green Zone – Safe). A tourniquet applied for less than 2 hours duration has negligible impact upon limb salvage rates and minimised risk when removed. Tourniquet application for less than 2 hours represents the optimal standard of care.
Tourniquet application greater than 2 hours in duration is associated with increased risk of permanent injury (Amber Zone – Unsafe). Nerve tissue and fast twitch muscle fibres are the most sensitive. Tourniquet application time represents a grey scale of increasing risk influenced by the pattern of wounding, tissue type, and other associated injuries.
Tourniquet time of greater than 4 hours is associated with progressively higher risk of significant permanent functional injury and failure of limb salvage procedures (Red Zone – Critical). Should the limb remain viable, increasing tissue damage will likely be sustained resulting in permanent injury and loss of function. Increasing health risks beyond the local limb effects are observed when the tourniquet is released.
Tourniquet application times greater than 6 hours remains a strong predictor of unsuccessful functional limb preservation and amputation is typically recommended (Black Zone – Terminal).
Arterial tourniquets when utilised correctly represent a highly effective life saving measure for the management of catastrophic haemorrhage due to penetrating limb trauma. Tourniquet application, reassessment, replacement, and conversion techniques are recommended in accordance with TCCC guidelines even if delayed evacuation to a surgical care is anticipated. In the context of the evolving future of ADF operations, the Tourniquet Traffic Light provides a simplified framework for the common understanding of the time dependent outcomes associated with limb tourniquet application by both commanders and health care providers.