Prolonged Field Care (PFC) doctrine within the Australian Defence Force (ADF) requires continual evolution to meet the challenges associated with operating within the limitations of tactical constraint, contested evacuation asset manoeuvre, conflicted access to evacuation assets, and extended evacuation distances.
In the management of catastrophic limb haemorrhage, extended duration tourniquet application time is associated with multiple technical and logistic consequences for both health care providers and commanders. Extended tourniquet ischaemia time results in both decreasing rates of functional limb preservation and increasing risks of systemic metabolic effects upon tourniquet release with reperfusion. A simplified framework for understanding the time dependent outcomes associated with limb tourniquet application has previously been presented as the Tourniquet Traffic Light.
Tourniquet Conversion (TC) involves the control of limb haemorrhage from penetrating injury by the application of local direct pressure, thereby enabling subsequent torniquet removal. From an operational perspective removing an arterial tourniquet permits potential de-escalation of triage and evacuation priorities thereby influencing mission support, the safety of retrieval service providers, and the allocation of local health resources.
From an injury management perspective early restoration of blood circulation improves the probability of functional limb preservation and reduces the risk of systemic metabolic reperfusion syndromes.
Utilisation of limb torniquets traditionally employs a binary approach – either the tourniquet is applied tightly to completely cease all distal blood supply or alternatively the tourniquet is removed completely by TC techniques. Tight and continuous arterial tourniquet application is entirely appropriate in most situations, such as when the anticipated transfer time to a surgical health care facility is relatively short (<2 hours), where adequate control of catastrophic limb haemorrhage is unable to be achieved by other means, or where the risk of further haemorrhage cannot be accepted in a hemodynamically unstable casualty.
Even in situations of complete arterial transection, however, the combined effects of arterial vasospasm, permissive systemic hypotension, and the local pressure applied by effective wound packing may often be enough to temporarily limit or significantly arrest further blood loss. Converting an arterial tourniquet in such situation, even if only intermittently or by partial release, may thereby enable distal limb perfusion by collateral vascular supply.
In the management of catastrophic limb haemorrhage where an extended duration of tourniquet application time is anticipated, Limited Tourniquet Conversion (LTC) may therefore be a viable alternative to provide both clinical and tactical advantages.
LTC introduces the concept that a Tourniquet Application State (TAS) may be considered as both dynamic and non-binary with continuous assessment and graduated movement between the extremes of full tourniquet application and complete removal according to clinical requirements (Figure 1). LTC represents an intermediate zone where an arterial tourniquet is utilised in a way to both control haemorrhage and to simultaneously enable distal perfusion to reduce local ischaemic limb damage and the risk of systemic reperfusion syndromes. The general features of LTC are presented in Table 1.
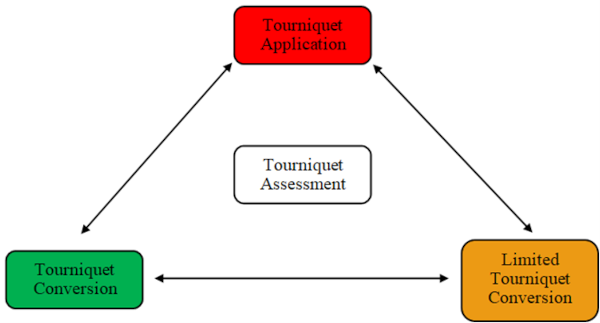
Figure 1: Conceptual framework of Tourniquet Application States in Prolonged Field Care.
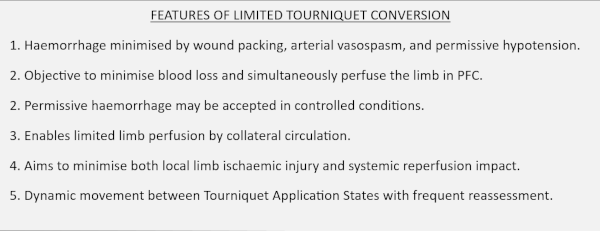
Table 1: Features of Limited Tourniquet Conversion.
LTC may be conducted by applying the tourniquet intermittently (Time Limited Tourniquet Conversion), by applying the tourniquet with reduced pressure (Pressure Limited Tourniquet Conversion), or by a combination of these techniques. The overarching principle of LTC is that whilst control of catastrophic limb haemorrhage takes priority (life over limb) this objective may be obtained by a combination of wound packing, permissive systemic hypotension, and arterial vasospasm with the tourniquet used as a dynamic augment device.
As the clinical and tactical environment changes, the Tourniquet Application State is adjusted to meet requirements. For example, with effective wound packing the control of limb haemorrhage may initially be achieved using a tourniquet applied at reduced pressures (Pressure Limited Torniquet Conversion) with distal limb perfusion observed via collateral circulation. After effective resuscitation measures and restoration of blood pressure, however, the resumption of bleeding may be detected and thereby necessitate full pressure tourniquet application to achieve appropriate haemorrhage control. For the duration of time where pressure limited tourniquet conversion was employed though, distal limb perfusion was observed, thereby providing potential improvement in clinical outcomes by minimising ischaemia.
Similarly, a casualty who has been managed by successful Tourniquet Conversion may resume significant bleeding when arterial vasospasm subsides, although this may be controlled by intermittently applying the tourniquet according to variations in blood pressure (Time Limited Tourniquet Conversion).
The key point is that all Tourniquet Application States require frequent reassessment.
LTC is an advanced technique suitable only for advanced health care providers. Multiple factors relating to the tourniquet, casualty, and operational environment need to be evaluated when considering the use of these techniques (Figure 2).
LTC is unnecessary if the total anticipated tourniquet time is less than 2 hours and is contraindicated where the limb distal to the tourniquet is clearly not viable or where traumatic amputation has occurred, particularly in the management of blast injury. Within an austere field environment, tourniquets should not be released after 2 hours of continuous of application due to the increasing risk of adverse metabolic and haemodynamic events upon limb reperfusion.
Likewise, due to potential haemorrhage risk upon tourniquet release, casualties should demonstrate relative haemodynamic stability prior to considering any tourniquet conversion. LTC should only be conducted by appropriately qualified health care providers where the tactical environment is suitable, including access to appropriate emergency resuscitative resources. How LTC is conducted will also be influenced by the experience and training of the individual health care provider.
For example, a health care provider with advanced anatomic acknowledge and surgical experience may consider augmenting local haemorrhage control measures with direct vessel ligation, thereby significantly influencing the requirement and nature of how a tourniquet is employed in PFC.
The benefits of LTC by either pressure or time limited techniques need to be balanced against the systemic side effects of potential blood loss in a resource limited austere environment. The minimum time duration for a reperfusion interval to provide worthwhile reduction in ischaemic risk is uncertain but is likely to be greater than 10 minutes.
The efficacy of a reperfusion interval will depend significantly upon the pattern of vascular injury, patency of any associated collateral arterial supply, and the general clinical state of the casualty. Time limited tourniquet conversion may be repeated every 2 hours to enable distal perfusion through collateral vasculature, providing the degree of blood loss associated with tourniquet release episodes is sufficiently minimised.
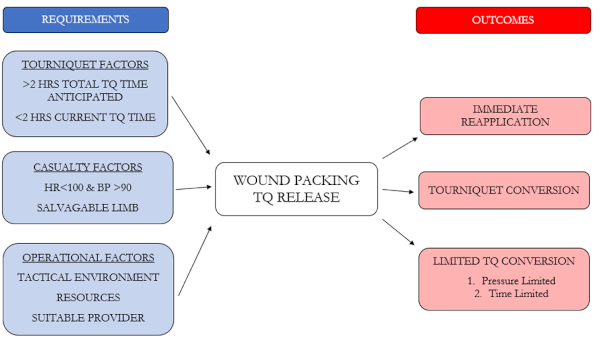
Figure 2: Technical conduct of tourniquet release and limited tourniquet conversion in prolonged field care.
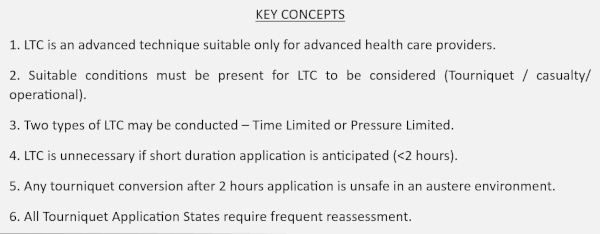
Table 2: Limited Tourniquet Conversion operational guidelines.
LTC represents an evolution of our traditional approach to tourniquet management within the ADF. The conduct of LTC whilst not without risk represents a necessary step in adapting healthcare delivery to meet the operational requirements of an evolving national defence environment.









