Previous articles published within The Cove have discussed a variety of topics relating to tourniquet application and their management in prolonged field care. This article connects a number of these concepts to provide a comprehensive overview of the training elements required to achieve Fundamental Level tourniquet de-escalation competency.
Tourniquet de-escalation refers to a spectrum of procedures and skills used to minimise or eliminate the harm associated with tourniquet ischaemia. In preparation for contested large-scale combat operations, the ADF requires tourniquet de-escalation capacity at scale, spread throughout the organisation. Tourniquet de-escalation may be organised into a three-tiered skill framework according to procedural complexity (Figure 1). Fundamental level tourniquet de-escalation includes a limited number of high impact knowledge tools and simple procedural skills, suitable for all soldiers to safely administer with appropriate training.
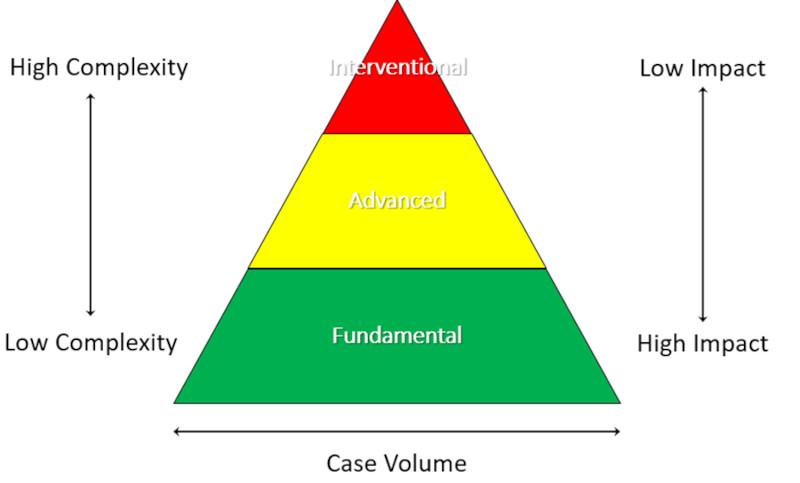
Figure 1: Tourniquet de-escalation framework. Fundamental de-escalation skills represent the highest value proposition from an organisational perspective, delivering high impact clinical and tactical outcomes to large numbers of casualties through the application of low complexity interventions.
All-corps Fundamental tourniquet de-escalation skills are organised into three phases: Assess, Convert, and Mitigate.
Phase 1 – Assess
The Tourniquet Traffic Light represents a tool for understanding safe tourniquet application times and the suitability for tourniquet conversion within an austere environment (Figure 2). The rule to remember is that tourniquet application and conversion is safest within the Green Zone (less than two hours). Limb tourniquets applied within the Green Zone are highly unlikely to cause ischaemic damage if approved devices and techniques are employed.
Therefore, if the casualty can be easily and reliably transported to a higher-level heath care facility within two hours of tourniquet application, then Tourniquet Conversion can potentially wait. If a time delay of greater than two hours is anticipated, however, field tourniquet de-escalation measures should be considered at the earliest suitable opportunity. If a tourniquet has been applied for greater than two hours though (outside Green Zone), conversion or replacement techniques represent high risk interventions that require advanced medical capability and should only be conducted by appropriately trained and equipped health care providers.
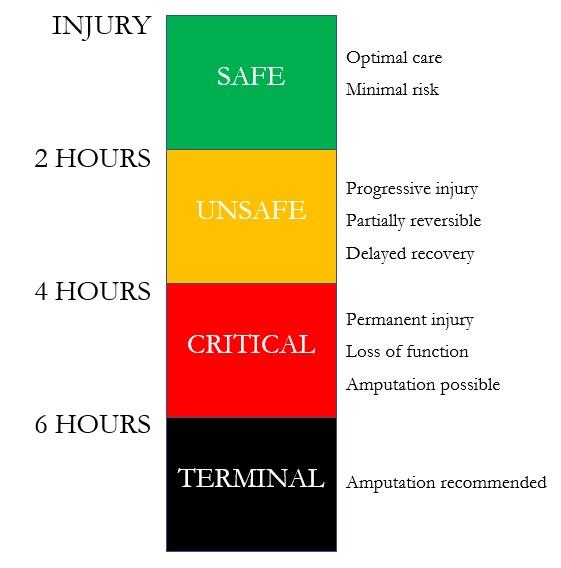
Figure 2: The Tourniquet Traffic Light. Tourniquet application and conversion within the Green Zone is associated with lowest risk.
Phase 2 – Convert
Tourniquet Conversion is the controlled release of an Immediate Action Tourniquet after the conduct of compression wound packing and the application of pressure dressings (Figure 3). Conversion represents ideal tourniquet de-escalation state as blood supply to the limb is restored. Conversion may be undertaken by following the all-corps Tourniquet Conversion-Replacement Drill, as previously described within The Cove.
Successful Tourniquet Conversion not only decreases the risk of limb injury but also provides significant tactical and operational advantages by enabling re-prioritisation of mobility assets and evacuation logistics.

Figure 3: Tourniquet Conversion. After compression wound packing and the positioning of a Deliberate Tourniquet directly to skin, 5cm above the wound, the Immediate Action Tourniquet is released. If no re-bleeding is observed, Tourniquet Conversion is considered successful.
Phase 3 – Mitigate
Mitigation measures are used where an arterial tourniquet cannot be removed. This may occur after unsuccessful Tourniquet Conversion or alternatively, where Tourniquet Conversion cannot be safely attempted due to a prolonged duration of application (greater than two hours) or if the casualty is in shock due to severe blood loss. Even though a tourniquet is still required, the harm associated with extended duration application times may still be minimised using mitigation measures.
Tourniquet Replacement involves the application of a second tourniquet at a level lower than the original Immediate Action Tourniquet when compression wound packing and pressure dressings alone are insufficient to control high volume bleeding (Figure 4). Tourniquet Replacement may be undertaken by following the all-corps Tourniquet Conversion-Replacement Drill, as previously described within The Cove. Replacing the tourniquet to a lower level not only reduces the extent of limb damage but also the generalised risk from exposure to toxic metabolites associated with limb ischaemia.

Figure 4: Tourniquet Replacement. Control of severe bleeding is obtained by the application of a Deliberate Tourniquet 5cm above the wound.
Where enduring tourniquet application is required for any duration, limb cryotherapy will reduce tissue metabolic rate and oxygen consumption and thus potentially improve limb viability for any given duration of tourniquet application. One method of obtaining limb cryotherapy in an austere setting is simply to expose the limb to the ambient environment. As the tourniquet prevents rewarming from blood circulation below the level of application, the tissues will spontaneously cool to ambient environmental temperature.
Where a hypothermia blanket has been applied to prevent central (core) hypothermia, the injured limb with tourniquet applied is therefore excluded from the wrap construct (Figure 5). Excluding the injured limb from the hypothermia wrap also enables regular monitoring of the wound, provides a visual alert to healthcare providers that a tourniquet has been applied, and facilitates wound care without disruption of the hypothermia wrap.

Figure 5: The Limb Exclusion Hypothermia Wrap. The injured limb with tourniquet applied is excluded from the hypothermia wrap construct to enable passive cryotherapy, serial observation, and wound management.










The observation of widespread iatrogenic harm from extended duration tourniquet application within the current Russo-Ukrainian conflict is driving a rethink of protocols and training world-wide. Evolution of tourniquet doctrine, whilst primarily being driven by military necessity, equally applies to civilian healthcare where greater than 2 hours of tourniquet application time is anticipated.
In terms of evolving tourniquet care standards in the United States, you may find these resources of interest:
1.https://wms.org/magazine/magazine/1424/Tourniquet-Replacement/default.aspx
2.https://journals.lww.com/jtrauma/fulltext/2023/12000/rethinking_limb_tourniquet_conversion_in_the.22.aspx
3.Tourniquets in TCCC Guidelines (Jan 2024) - Deployed Medicine