The application of arterial tourniquets is fundamental for the management of catastrophic limb haemorrhage resulting from penetrating trauma. Offsetting the liberal application of arterial tourniquets within the initial phases of Tactical Combat Casualty Care (TCCC), subsequent early reassessment with conversion or distal replacement is recommended where applicable, particularly within the first two hours of tourniquet application.
Recent articles relating to extended duration tourniquet application within The Cove have described the time dependent nature of ischaemic damage (Tourniquet Traffic Light), methods to reduce tissue injury associated with extended duration tourniquet application (Limb Exclusion Hypothermia Wrap; Limited Tourniquet Conversion in Prolonged Field Care), and the risks associated with limb reperfusion in prolonged field care (Tourniquet Conversion in an Austere Environment). These principles primarily relate to extended duration tourniquet management within a pre-hospital limited resource environment.
This article moves forward within the land-based trauma system to address aspects of the initial resuscitative management where adequate resources are now available to consider releasing a tourniquet after an extended duration of tourniquet application has elapsed (2-6 hours) in a casualty with an otherwise potentially viable limb.
Reperfusion following extended duration tourniquet application
There are multiple scenarios where timely tourniquet conversion is unable to be conducted safely in a field environment. Valid reasons to keep a tourniquet applied include significant vascular injury with resumption of catastrophic haemorrhage upon release, significant haemodynamic instability with insufficient resuscitative resources to risk further compromise, or the lack of appropriately skilled health care providers for the conduct of tourniquet conversion.
In these scenarios, maintenance of arterial tourniquet application, whilst a useful strategy, also carries negative consequences. Tourniquet associated limb ischaemia is a complex problem to manage in Prolonged Field Care (PFC), increasing in significance relative to the duration of time to definitive care. Reperfusion syndromes upon tourniquet release are associated with potentially life-threatening consequences, particularly when extending beyond 2 hours of warm ischaemia time (Figure 1).

Figure 1 / Risks associated with reperfusion of a severely ischaemic limb and underlying pathologic mechanisms
Acknowledging that reperfusion injury potentially undermines the management of an already compromised casualty, the overarching objective is that tourniquet release needs to be appropriately timed in relation to resuscitation. The guiding principles balancing resuscitation and tourniquet release are presented in Figure 2, with further description following.
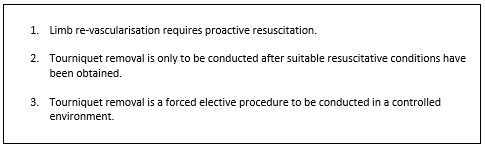
Figure 2 / Principles of resuscitation in preparation for ischaemic reperfusion after an extended duration of tourniquet application (2-6 hours)
- Limb re-vascularisation requires proactive resuscitation. Initial reperfusion of a blood depleted ischaemic limb with altered sympathetic tone results in hypotension due to volume sequestration, compounded by a reduction in pain mediated vasopressor activity. Immediate hypotension should be anticipated upon arterial torniquet removal even if further external blood loss is not observed. Simultaneously, the venous blood returning from a reperfused ischaemic limb is typically cold and acidotic with cellular injury leading to high concentrations of potassium and myoglobin. Proactive resuscitation measures to manage the predictable volumetric, cardiac, and renal aspects of torniquet removal after prolonged application are therefore recommended. Resuscitation efforts directed at minimising the systemic metabolic impact of tourniquet release should be undertaken prior to tourniquet removal.
- Tourniquet removal is only to be conducted after suitable resuscitative conditions have been obtained. Where other immediately reversible injuries exist, appropriate sequencing of damage control surgery will typically dictate tourniquet removal to be conducted only after appropriate control of abdominal and thoracic haemorrhage has been achieved and appropriately suitable haemodynamic reserve has been obtained.
- Tourniquet removal is a forced elective procedure to be conducted in a controlled environment. Whilst early tourniquet removal may re-establish distal limb perfusion and minimise the metabolic consequences of reperfusion, situational awareness in relation to the suitability of the health care facility and the tactical environment is required to manage the immediate and potentially life-threatening consequences of tourniquet release. Appropriate environmental conditions include consideration of monitoring equipment, resuscitative capability, surgical capability, and the skill sets of health care staff attending. Where suboptimal conditions exist, the risk of tourniquet release must be weighed against the consequences of extending tourniquet application times to first achieve better environmental conditions.
The Reperfusion Toolbox
The Reperfusion Toolbox is a series of resuscitative measures aimed at reducing the systemic consequences of ischaemic limb reperfusion (Figure 3). These measures are recommended to be undertaken prior to tourniquet removal to stay ahead of resuscitative care requirements. Not all aspects of the Reperfusion Toolbox will be required in every case. These recommendations are intended as a guidance framework to assist clinicians in the recognition and management of important features of resuscitation during ischaemic limb salvage procedures. Individual clinical evaluation and judgement is therefore recommended.
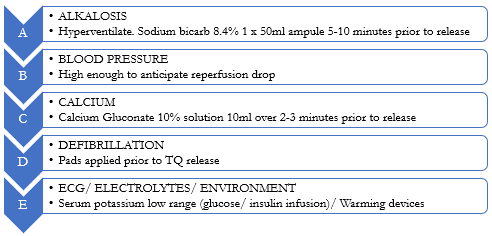
Figure 3 / The Reperfusion Toolbox (ABCDE)
A more detailed description of each step in the Reperfusion Toolbox is detailed below:
Alkalosis: Creation of mild respiratory and metabolic alkalosis by a combination of hyperventilation (if mechanically ventilated) and intravenous sodium bicarbonate infusion (0.5-1 mmol/kg or 1 ml/kg of 8.4% w/v sodium bicarbonate. The typical adult dose of bicarbonate to be considered is 1 x 50ml ampoule of 8.4% sodium bicarbonate), administered 5-10 minutes prior to tourniquet release. Minimising metabolic acidosis in a poly traumatised casualty is important in consideration of cardiac dysfunction and blood coagulopathy. Urinary alkalosis together with adequate hydration status and adequate urine output rate reduces the renal impact of myoglobinuria.
Blood Pressure: Systolic pressures are to be suitably managed in anticipation of a rapid and potentially significant decrease associated with ongoing haemorrhage, loss of pain mediated pressor activity and volume sequestration within the limb compounded by nerve ischaemia mediated sympathetic vasomotor dysfunction.
Calcium: Calcium Gluconate (10mls of 10% solution over 2-3 minutes IV) to provide a cardiac stabilising effect in consideration of dysrhythmia due to hyperkalaemia. Associated role in the management of critical haemorrhage associated coagulopathy.
Defibrillation: Defibrillation pads applied prior to tourniquet release with crash trolley on standby.
Electrolytes: Serum potassium ideally placed into low normal range (approximating 3.5 mmol/L) prior to tourniquet removal. Consider dextrose insulin infusion (10 Units in 50ml of 50% solution over 2-3 minutes IV) for active reduction in serum potassium levels.
Electrocardiography: Continuous electrocardiography monitoring in place for the early detection of hyperkalaemic dysrhythmia.
Environment: In anticipation of progressive compromise of hypothermia management, institution of regular (core) temperature monitoring, environmental temperature control with forced air warming devices, and fluid warming.
Summary
Reperfusion injury after extended duration tourniquet application represents a significant threat to effective resuscitation. Tourniquet release after application times greater than 2 hours should be conducted with situational awareness of the negative clinical impacts of reperfusion, suitability of the health care facility, and the tactical environment. The Reperfusion Toolbox represents a recommended series of healthcare measures employed to reduce the risks associated with tourniquet release after 2-6 hours of warm ischaemia.
Acknowledgement
Manuscript developed with the assistance of Dr Nathan Peters (Anaesthetist, Wesley Anaesthesia and Pain Management, Brisbane Australia).









